Pharmacogenetics – what a psychiatrist should know
- Marit Tveito

- Dec 7, 2025
- 4 min read
Interview with Elvira Bramon, Professor of Neuroscience and Mental Health
Marit Tveito talks with Elvira Bramon, Professor of Neuroscience and Mental Health at University College London, about what psychiatrists should know when integrating pharmacogenetic insights into everyday clinical decision-making. Their conversation sheds light on current evidence, practical challenges, and the future role of genetics in mental health care.
Marit Tveito: In plain words – what is pharmacogenetics?
Elvira Bramon: Pharmacogenetics is the study of genetic influences on medication response. Pharmacogenetic (or pharmacogenomic) tests can be used to tailor treatment to an individual, based on their likely response to a particular drug or to a group of drugs.
What should psychiatrists know about pharmacogenetics?
In psychiatry, we use empirical prescribing, just like all other areas of medicine do. However, we have a ‘luxury problem’ with over 40 different drugs licensed to treat common conditions like depression and psychosis. Finding a suitable drug and dose is not trivial and it can take multiple cycles of prescribing, adjusting and switching. Pharmacogenetic information could help to optimise the prescribing of mental health medications. This is important given that many of our patients take their psychotropic drugs for long periods of time.
How do you think genetic testing can help improve the treatment of mental disorders?
Recent studies such as the multi-centre PREPARE trial show that pharmacogenetic testing can bring considerable reductions in adverse drug reactions across many drugs commonly used in medicine (Swen et al, 2023). A sub-analysis focusing on antidepressant and antipsychotic drugs confirmed encouraging findings too with reductions in both side effects and hospitalisations, when they used pharmacogenetics (Skokou et al, 2024).
What are the possible barriers for use in clinical practise?
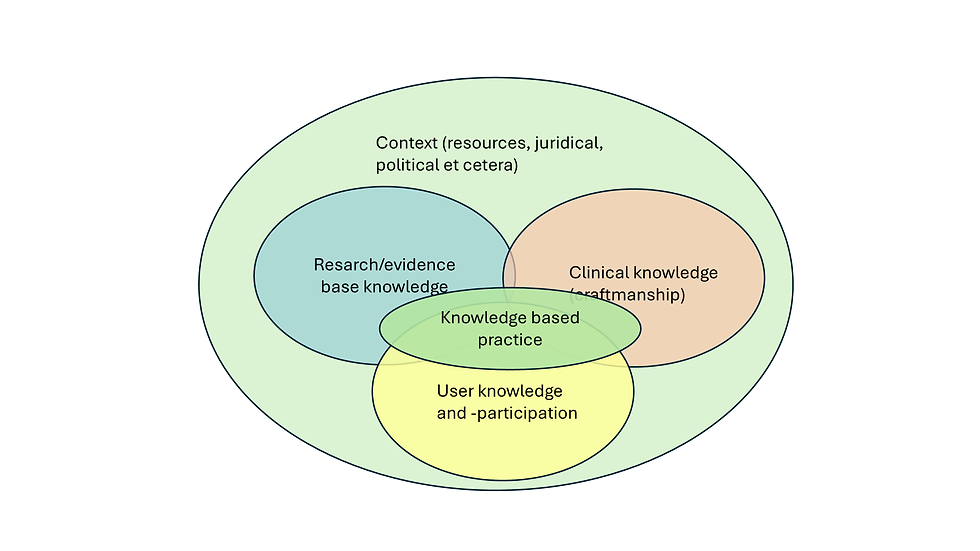
We have done a survey of 120 UK mental health prescribers mostly psychiatrists. Over 70% of them said pharmacogenomics is relevant to their clinical practice. However, they also reported they lack training in genomics. Most centres providing mental health care around the world do not have access to laboratories offering pharmacogenetic testing. There is a risk of building unrealistic expectations about pharmacogenetic tests; we need to continue to promote evidence-based pharmacogenomic interventions and holistic prescribing.
Have you had any experiences with how the patients respond to genetic testing for guiding treatment?
Yes, we also did a survey of people with psychosis who had experienced pharmacogenetics testing as part of our project GEMS (Genetics and Environment in Mental health Study). Their feedback was encouraging and positive. Some people found the information complex and asked for more accessible formats. Many patients said the test was useful and that it helped them make decisions about their treatment with their clinicians more collaboratively (Richards-Brown et al, 2025).
There is growing interest amongst the public about genomics. People are getting tested through direct-to-consumer labs and bring their pharmacogenetics report to our clinics. As psychiatrists will need to be ready to provide advice and embrace genomics medicine.

Where are the knowledge gaps in the field of pharmacogenetics in psychiatry? And how can these gaps be filled?
In most countries around the world there are gaps in training of clinicians and limited access to laboratories with pharmacogenetic capabilities.
The field is advancing rapidly and there are evidence-based guidelines such as CPIC and DPWG. These cover antidepressants very well, where multiple randomised controlled trials have been completed (Fares-Oter et al, 2025; Milosavljević et al, 2024). There are also some studies on pharmacogenetics testing for antipsychotics (Saadullah Khani et al, 2024). Important drugs in our speciality like Lithium and Clozapine don’t have pharmacogenetic guidelines yet. We are finalising a new guideline for ACKR1 genetic testing for people taking clozapine, as part of the Centre of Excellence in Regulatory Science and Innovation at the University of Liverpool.
Because genetic variants affecting drug response are relatively rare, we will need very large samples. These are best achieved through naturalistic pharmacogenetic studies linked to electronic health records, to other registers and to biobanks. The Nordic registers will be invaluable.
Do you have any advice to Nordic psychiatrists who are interested in using pharmacogenetic testing and wish to learn more?
There is already great expertise in this field in Norway. For example, at the Center for Psychopharmacology in Diakonhjemmet Hospital in Oslo, more than 10 000 patient samples are analysed every year. The tests are also available in three other hospital laboratories in Norway, resulting in good availability for both general practitioners and hospital specialists.
Norway is one of the few countries in the world that has already implemented a nation-wide web-based tool for guidance in pharmacogenomic testing in mental health as well as other areas. The tool offers clinicians detailed information for genetics-guided prescribing of a wide range of psychotropic medicines as can be seen in this link https://cypinfo.no/.
In the UK, we have not yet implemented pharmacogenomics in mental health care, but this area is developing rapidly. The UK’s National Genomics Education Programme GeNotes offers brief ‘in the clinic’ articles for clinicians and a more in-depth knowledge hub. GeNotes covers genomic medicine across multiple specialities including pharmacogenomics as well as a mental health. New articles and updates are regularly published in this open access resource: https://www.genomicseducation.hee.nhs.uk/genotes/.
At the GeNotes team we welcome your suggestions for new topics in pharmacogenomics for mental health.
Thank you for the conversation. □